Today we are going to talk about Omalizumab. So this is it, the last post on this long journey into the microbiology world. And I mean we have talked about a lot we’ve talked about our favorite topics, vaccines, to go going epidemics in other parts of the world to the ongoing epidemic that is happening in our very lives today. Our last topic has to do with antibodies. But not just any, we are going to talk about monoclonal antibodies. What is this you ask? Well deep breaths I’ll explain and I’ll even talk to you about a specific one and what it does to you.
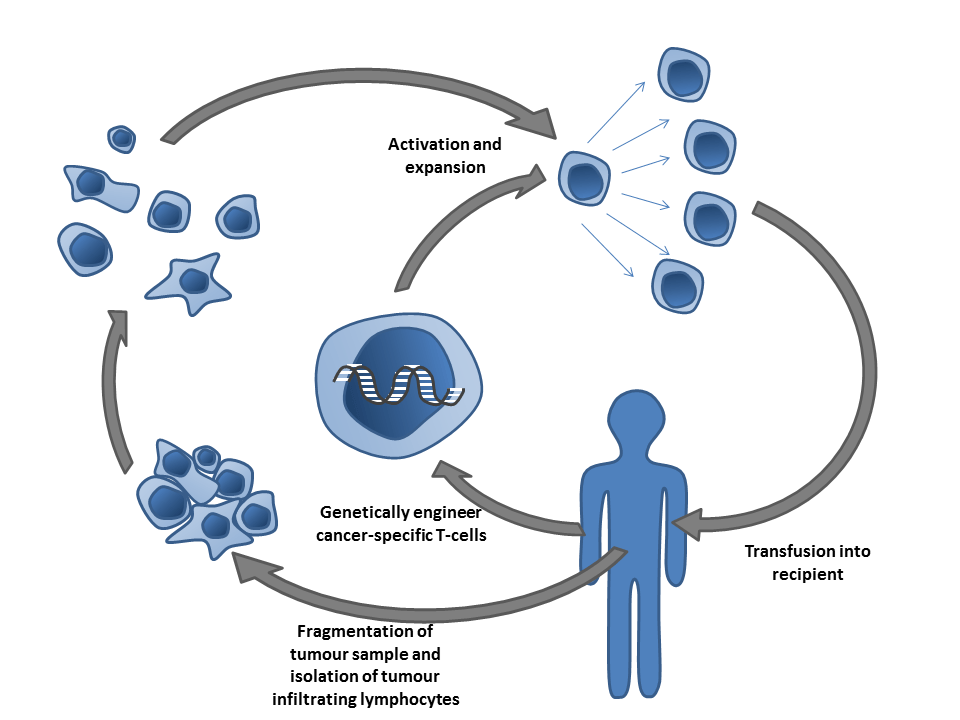
So what exactly are Monoclonal Antibodies?
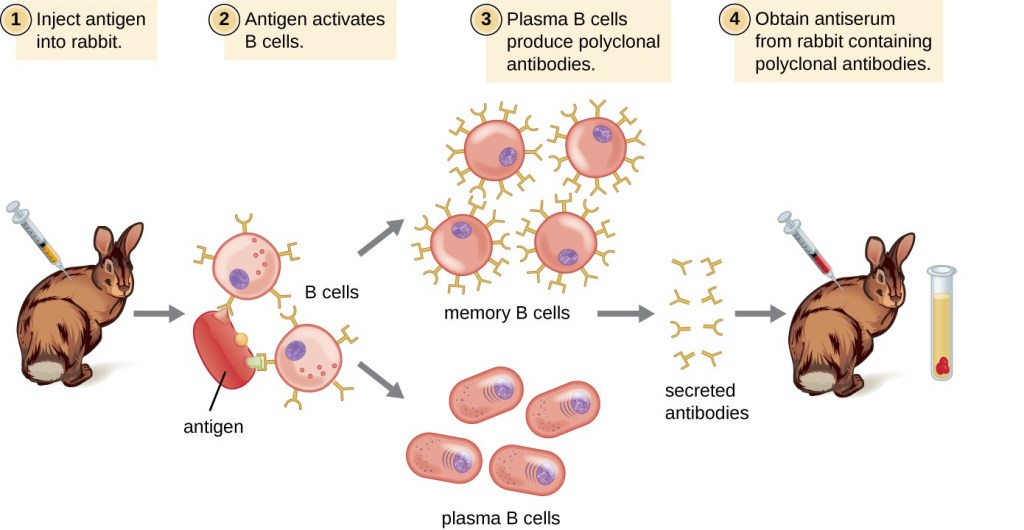
From our previous conversations we know that our body makes its own antibodies right? We’ve talked about IgM and IgG specifically but we also mentioned how there is a IgD, IgE and IgA. All of which respond in their own way in the body providing protection against invaders. But we also know how technology is always changing and because of so scientists can now do many things. According the Medicinenet, scientists can now make antibodies similar to those made body and can even make them act in similar ways of the antibodies in the body. The way they do this is clone immune cells and make those clones produce antibodies. These antibodies then bind to one antigen. This is why they are called monoclonal because they bind to one antigen. Now there are such things are polyclonal antibodies which are clones of multiple immune cells that synthesize antibodies and these antibodies can bind to multiple antigens. But today we will just focus on monoclonal antibodies. Next, we are going to talk about a drug that works by having monoclonal antibodies.
Omalizumab
Aka it’s brand name, Xolair. In general (via Wikipedia) this drug works to reduce allergic sensitivities and can also be used to control severe allergic asthma that is hard to control with other treatments such as corticosteroids. So essentially this drug helps people’s allergies chill out when they start to go crazy. And we will discuss how it does this. So how does it really work? So we have to start by talking about how our immune response works to be able to talk about how this drug works to counter that reaction.
Allergic Reactions
When an invader enters the body there are many paths that can happen in response to said invader entering the body. One of these paths is that the invader is taken up by APCs which are Antigen presenting cells. APCs then take the antigen and show it to T-Cells which helps activate T-Cells who then go along to activate B-Cells. When B-Cells are activated they differentiate into plasma cells. These plasma cells undergo a thing called class switching and affinity maturation where they become better cells with stronger receptors to bind to, also during this process they are told which antibody they are supposed to produce and release. When there is an antigen that is classified as an allergen B-Cells are told to make IgE. When IgE is released they then go to bind onto IgE receptors on other cells, such as basophils and mast cells. When they bind they cause the mast cells to activate and release histamine. This release of histamine is what causes your normal side effect in allergic reactions, such as hives that cause the redness, itching, burning or stinging. Like we learned in class the activation and actions of B-Cells are part of the immune system that requires more specific responses meaning that this is a part of the acquired immune system because of all of the activation signaling. (Information from Lecture, The textbook and the NCBI)
Our Drug
So now we know exactly how our body responds to an allergen we can fully understand how our drug works. So for our drug to lower allergic reactions according to the Indian Journal of Dermatology, our drug works against IgE. Which we know makes this sense because IgE causes the release of Histamine which causes our severe allergic reaction. So working against IgE makes sense. In order to do this it works by binding to free IgE. Our drug has a greater affinity of binding IgE than IgE does to binding to other cells. Meaning it’s easier for our drug to bind and holds on tighter to IgE than IgE would with other cells. Now our drug doesn’t bind to IgE that is already bound to other cells, but only free IgE. Which makes sense when like you think about it because the drug doesn’t stop an allergic reaction just reduces the severity of it. So to reduce the severity if we reduce the amount of IgE that can bind we can reduce the amount of histamine that will be released. This drug works by interacting with the products of the acquired immune system when it interacts with free IgE floating around.
Other sources such as medicinenet, says that our drug works by binding to the receptors on the cells that IgE would bind to instead of the IgE itself. Either way it’s lowering/preventing the chemicals that would be released by the cells activated by IgE.
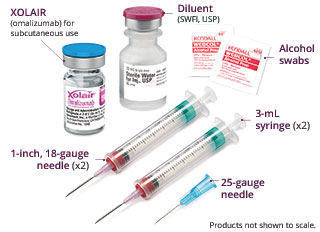
The Down Side
According to medicinenet the side effects are as follows:
- Headaches
- Viral Infections
- Upper Respiratory Tract Infections
- Injection-site reactions such as:
- Pain
- Redness
- Swelling
- Itching
- Bruising
- More Serious Side Effects include:
- Difficulty breathing
- Fainting
- Low Blood Pressure
- Swelling of the Tongue
They also reported that taking this drug made patients more susceptible to cancer.
So yeah that’s about everything. I know this blog was a lot longer than usual but it does give a lot of information. Information which could be helpful if you have severe asthma/allergic reactions. And if not then at least you have…jeopardy knowledge. I hope you have learned a thing or two throughout our microbiology journey. I know I have. If you have made it this far, thanks for reading!